March 2021
3/22/2021 | BY Rubini Pathy, MD FRCSC
5 Tips for Diagnosing and Managing a SCFE
- Disruption of the proximal femoral physis
- Anterior displacement and external rotation of the proximal femoral metaphysis with variable posterior displacement of the epiphysis, which remains in the acetabulum (1)
- rare subtype: “valgus slip”: antero-medial neck translation & posterovalgus inclination of the femoral head (1)

- rare subtype: “valgus slip”: antero-medial neck translation & posterovalgus inclination of the femoral head (1)
- Anterior displacement and external rotation of the proximal femoral metaphysis with variable posterior displacement of the epiphysis, which remains in the acetabulum (1)
- Most common hip disorder in adolescents (1 to 100 per 100, 000) (2)
- Affects Boys > Girls (1.5:1) (3.4)
- Average Age of onset:
- Boys: 12.7 to 13.5 y.o (3,4)
- Girls: 11.2 to 12 y.o (3,4)
- Bilateral slip: 20 to 80%5 – usually asynchronous
- Pathophysiology
- Mechanical overloading of a healthy physis
- Obesity (6)
- Anatomic characteristics
- Femoral or acetabular retroversion (7,8)
- Increased obliquity of the proximal femoral physis (9,10)
- Normal loading of a weak physis
- Endocrine or other underlying disorders
- Consider when age < 10 y.o or > 16 y.o or if BMI < 50th percentile
- Endocrine or other underlying disorders
- Mechanical overloading of a healthy physis
- Other risk factors
- Ethnicity: Black / Native American / Hispanic > White (3)
- Seasonal variations: higher incidence in summer (11)
- Regional: USA - higher incidence in the Northeast and West (3,11)
2. DIAGNOSING A SCFE – KEY POINTS: CLINICAL PRESENTATION
- History
- Age
- Groin, thigh or knee pain – acute vs. chronic vs. “acute-on-chronic”
- Limp – with or without pain
- Ability to weightbear with or without crutches (Loder Classification) (12)
- Stable: able to WB (~10% risk of AVN)
- Unstable: unable to WB (up to 50 % risk of AVN)
- NB: Loder clinical classification may not correlate with intra-op stability (13)
- 29% of clinically stable slips were unstable intra-op
- Ability to weightbear with or without crutches (Loder Classification) (12)
- o +/- history of trauma
- **** Diagnosis is often delayed: Average time from first physician visit to diagnosis (14)
- 94 days (non-ortho provider) vs. 2.9 days (ortho provider)
- Significant delay if knee pain was presenting symptom (110 days vs 59 days: presentation to dx)
- Physical Examination
- External foot progression angle
- “Obligate external rotation”
- Hip externally rotates when assessing hip flexion
- Limited hip internal rotation
- BMI
- Imaging
- Supine AP Pelvis and bilateral frog leg views
- ID slip & Quantify severity of slip (see xray examples below)
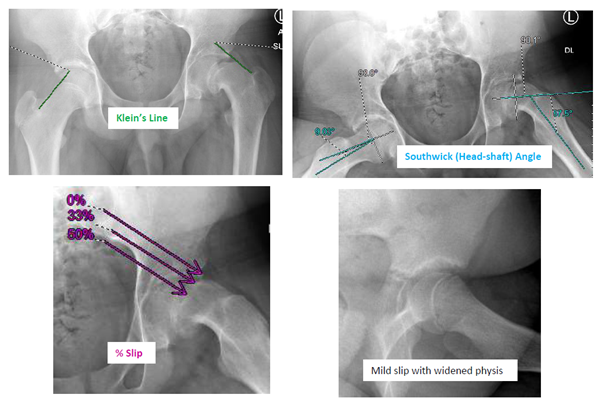
- Klein’s line on AP
- Line along superior femoral neck should normally intersect the epiphysis
- Southwick (Head-Shaft) Angle on frog leg lateral (1)
- Angle between the femoral shaft and a line perpendicular to the epiphysis
- This angle is then subtracted from the contralateral normal hip
- In bilateral SCFE: subtract 10 degrees
- Mild (0–30°), moderate (30–60°), or severe (> 60°)
- % slip: how much the metaphysis has slipped on the epiphysis
- Mild: neck displaced < 1/3 diameter of the epiphysis, Moderate: 1/3 to ½; Severe: > ½
- “Pre-slip”: Widening or irregularity of physis may be the only sign (MRI may be helpful)
- CT / MRI useful if planning a surgical hip dislocation
- Klein’s line on AP
3. MANAGEMENT GOAL & OPTIONS
- GOAL
- STABILIZE the slip to
- MINIMIZE THE RISK OF AVN
- PREVENT FURTHER DEFORMITY
- Existing and further deformity can cause femoro-acetabular impingement, intraarticular cartilage and labral injury, symptomatic degenerative osteoarthritis
- Eliminate pain
- STABILIZE the slip to
- OPTIONS
- In situ pinning
- Most common technique
- Stabilize the slip with no attempt to correct the current deformity
- May require future surgery for symptomatic deformity correction
- Surgical hip dislocation with acute correction of deformity (Modified Dunn osteotomy) and stabilization of slip (15,16)
- Option in high volume centers with experienced surgeons to minimize the moderate risk of AVN
- Open reduction and stabilization (17): described in one center
- In situ pinning
- In situ pinning
- Might get “serendipitous” reduction
- No attempt at closed reduction
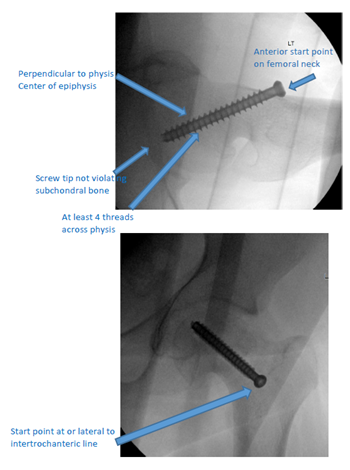
- Anterior start on femoral neck
- At or lateral to the intertrochanteric line
- To avoid impingement with ROM
- At or lateral to the intertrochanteric line
- Cannulated 6.5 / 7.3 mm screw
- Screw placed perpendicular to physis, center of epiphysis
- At least 4 threads across physis (in epiphysis)
- Do not violate subchondral bone
- “approach-withdraw” test using fluoroscopy
- screw tip should at least 5 mm from subchondral bone on all views
- Post-operative care
- Usually protected WB if unstable, WBAT if stable
- Follow up until physeal closure
- At follow up visits: always ask about symptoms on the side of the slip and contralateral hip / thigh / knee pain
- On follow-up AP and bilateral frog leg xrays, look for
- Slip progression
- Chondrolysis (narrowing of joint space < 3 mm, usually due to screw penetration)
- AVN
- Screw tip position and # of threads across physis
- Contralateral slip
- Complications arising from the deformity – FAI
- Prophylactic pinning of contralateral hip
- Controversial (18,19)
- Relative Indications
- Age : Boys < 12, Girls < 10
- Underlying disorder (Endocrinopathy / radiation)
- Poor follow-up potential
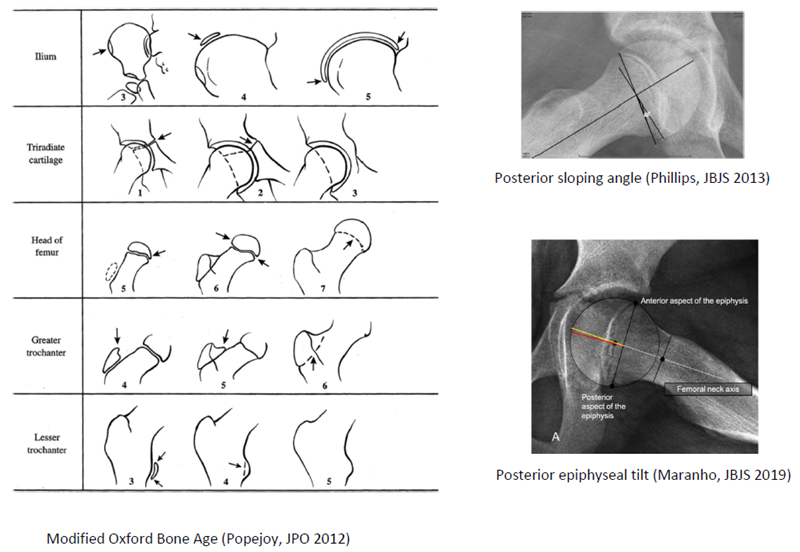
- Modified Oxford Bone Age Score 16-18 or open tri-radiate (20)
- Posterior sloping angle > 14 ° (21)
- Posterior epiphyseal tilt > 10 ° (22)
- Single vs. Multiple screws
- Controversial
- Consider for unstable, displaced hips: 66% stronger fixation with 2 screws (23)
- Decreased complication rate with one screw (24)
- 1 screw = 4.6%, 2 screws = 19.6%, 3 screws = 36%
- Single screw fixation is 77% as stable as double screw fixation
- Complications
- AVN
- Chondrolysis
- Peri-implant fracture
- Progression of slip
- Residual proximal femoral deformity limiting ROM or causing FAI
- Leg length discrepancy
- Degenerative OA
- Contralateral slip
REFERENCES
1. Millis MB. SCFE: clinical aspects, diagnosis, and classification. J Child Orthop. 2017;11:93–8.
2. Novais EN, Millis MB. Slipped capital femoral epiphysis: prevalence, pathogenesis, and natural history. Clin
Orthop Relat Res.2012;470:3432–8.
3. Lehmann CL, Arons RR, Loder RT, Vitale MG. The epidemiology of slipped capital femoral epiphysis: an update. J
Pediatr Orthop. 2006;26:286–290.
4. Loder RT. The demographics of slipped capital femoral epiphysis. An international multicenter study. Clin Orthop
Relat Res. 1996;322:8–27.
5. Loder RT, Aronson DD, Greenfield ML. The epidemiology of bilateral slipped capital femoral epiphysis. A study of
children in Michigan. J Bone Joint Surg Am. 1993;75:1141–1147.
6. Manoff EM, Banffy MB, Winell JJ. Relationship between bod ymass index and slipped capital femoral epiphysis. J
Pediatr Orthop. 2005;25:744–6.
7. Gelberman RH, Cohen MS, Shaw BA, Kasser JR, Griffin PP, Wilkinson RH. The association of femoral retroversion
with slipped capital femoral epiphysis. J Bone Joint Surg Am. 1986;68:1000–1007
8. Ezoe M, Naito M, Inoue T. The prevalence of acetabular retroversion among various disorders of the hip. J Bone
Joint Surg Am. 2006;88:372–379
9. Mirkopulos N, Weiner DS, Askew M. The evolving slope of the proximal femoral growth plate relationship to
slipped capital femoral epiphysis. J Pediatr Orthop. 1988;8:268–273.
10. Pritchett JW, Perdue KD. Mechanical factors in slipped capital femoral epiphysis. J Pediatr Orthop. 1988;8:385–
388.
11. Loder RT. A worldwide study on the seasonal variation of slipped capital femoral epiphysis. Clin Orthop Relat
Res. 1996;322:28–36.
12. Loder RT, Richards BS, Shapiro PS, Reznick LR, Aronson DD. Acute slipped capital femoral epiphysis: the
importance of physeal stability. J Bone Joint Surg Am. 1993;75:1134–40.
13. Ziebarth K, Domayer S, Slongo T, Kim YJ, Ganz R. Clinical stability of slipped capital femoral epiphysis does not
correlate with intraoperative stability. Clin Orthop Relat Res 2012;470:2274-2279.
14. Hosseinzadeh P, Iwinski HJ, Salava J, Oeffinger D. Delay in the Diagnosis of Stable Slipped Capital Femoral
Epiphysis. J Pediatr Orthop. 2017 Jan;37(1):e19-e22.
15. SankarWN,Vanderhave KL, Matheney T, Herrera-Soto JA, Karlen JW. The modified Dunn procedure for unstable
slipped capital femoral epiphysis. J Bone Joint Surg Am. 2013;95:585–91.
16. Upasani VV, Matheney TH, Spencer SA, Kim Y-J, Millis MB, Kasser JR. Complications after modified Dunn
osteotomy for the treatment of adolescent slipped capital femoral epiphysis. J Pediatr Orthop. 2014;34:661–7.
17. Parsch K, Weller S, Parsch D. Open reduction and smooth Kirschner wire fixation for unstable slipped capital
femoral epiphysis. J Pediatr Orthop. 2008;29:1–8.
18. Kocher MS, Bishop JA, Hresko MT, Millis MB, Kim YJ, Kasser JR. Prophylactic pinning of the contralateral hip after
unilateral slipped capital femoral epiphysis. J Bone Joint Surg Am. 2004 Dec;86(12):2658-65.
19. Schultz WR, Weinstein JN, Weinstein SL, Smith BG. Prophylactic pinning of the contralateral hip in slipped capital
femoral epiphysis : evaluation of long-term outcome for the contralateral hip with use of decision analysis. J
Bone Joint Surg Am. 2002 Aug;84(8):1305-14.
20. Popejoy D, Emara K, Birch J. Prediction of contralateral slipped capital femoral epiphysis using the modified
Oxford bone age score. J Pediatr Orthop. 2012 Apr-May;32(3):290-4.
21. Phillips PM, Phadnis J, Willoughby R, Hunt L. Posterior sloping angle as a predictor of contralateral slip in slipped
capital femoral epiphysis. J Bone Joint Surg Am. 2013 Jan 16;95(2):146-50.
22. Maranho DA, Ferrer MG, Kim YJ, Miller PE, Novais EN. Predicting Risk of Contralateral Slip in Unilateral Slipped
Capital Femoral Epiphysis: Posterior Epiphyseal Tilt Increases and Superior Epiphyseal Extension Reduces Risk. J
Bone Joint Surg Am. 2019 Feb 6;101(3):209-217.
23. Kishan S, Upasani V, Mahar A, Oka R, Odell T, Rohmiller M, Newton P, Wenger D. Biomechanical stability of
single-screw versus two-screw fixation of an unstable slipped capital femoral epiphysis model: effect of screw
position in the femoral neck. J Pediatr Orthop. 2006 Sep-Oct;26(5):601-5.
24. Karol LA, Doane RM, Cornicelli SF, Zak PA, Haut RC, Manoli A 2nd. Single versus double screw fixation for
treatment of slipped capital femoral epiphysis: a biomechanical analysis. J Pediatr Orthop. 1992 Nov-
Dec;12(6):741-5.
