July 2020
7/6/2020 | BY Craig Louer, MD, POSNA Resident Communications Committee
5 Things to Know to Help Understand Pediatric Pelvic Osteotomies
The most commonly used and tested osteotomies can be grouped and categorized in a multitude of ways, but the framework below has worked well for me. This organization allows you to group by common technical details and get insight into what the osteotomy is designed to do.
- Re-directional osteotomies involve freeing a segment of the pelvis around the acetabulum to allow the acetabulum to be reoriented in space without changing its structure/shape.
- Re-shaping osteotomies are incomplete osteotomies that “hinge” on the triradiate cartilage, therefore adding coverage but also reducing volume of the acetabulum.
- Salvage osteotomies are used to attain coverage in situations where an articular surface cannot be simply re-oriented or re-shaped into position: these use bone graft or ilium (covered in capsule) to provide structural support/coverage.
| Re-directional Osteotomies |
|
| Re-shaping Osteotomies (“Acetabuloplasty”) |
|
| Salvage |
|
2. Re-directional Osteotomies: When & Where?
The single innominate (Salter), triple innominate (Steel), and Bernese PAO (Ganz) are the most common re-directional osteotomies, with differing indications and use depending mostly on age of patient. The Salter and Steel osteotomies are used in skeletally immature patients, with the Ganz osteotomy being of use in mature patients with closed tri-radiate cartilage.
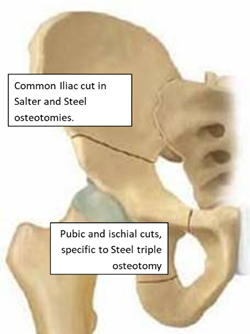
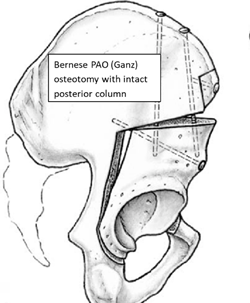
The Salter osteotomy is common in infantile DDH but is rarely used above age 8. At that point, the Steel triple osteotomy is more popular, with indications still for dysplasia and Perthes Disease. Both involve a supra-acetabular ilium cut, with the difference being the “hinge-point” medially: the Salter has no medial cuts and hinges at the pubic symphysis while the Steel has ischial and pubic bone cuts to help better mobilize the segment in a more mature child. Both of these osteotomies avoid cuts through the tri-radiate cartilage, which is the differentiating factor from a Ganz PAO. The Ganz PAO has a “retroacetabular” cut that allows freeing of the acetabular fragment while sparing the posterior column structural support. Because this cut goes through where the tri-radiate cartilage would be, this is only done in mature patients who do not have ongoing acetabular growth and development.
3. Re-shaping Osteotomies: How are they different?
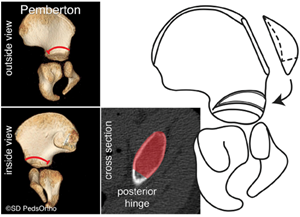
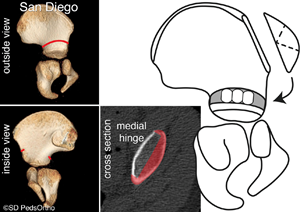
The Pemberton and Dega osteotomies are primarily used in immature patients with hip dysplasia: both idiopathic DDH as well as neuromuscular dysplasia. Both of these osteotomies reduce the volume of the acetabulum, which can help with congruency in some patients but should be avoided if the acetabular volume is already small. There is still quite vigorous debate over uses (and even the technical details) of these osteotomies and their modifications, so recognize that some may disagree with my “facts”, although this account is consistent with testing for trainees.
The Pemberton osteotomy is an incomplete osteotomy of the supra-acetabular ilium that goes through the inner and outer tables until stopping short of the sciatic notch and hinging upon the posterior tri-radiate cartilage. Because of its posterior hinge-point, the Pemberton obtains anterior-lateral coverage predominantly, although proponents argue they can alter it to obtain more global coverage. The Dega osteotomy (not pictured) has less disruption of the inner table and theoretically allows more lateral coverage. The differences between these two are subtle and quite possibly not clinically relevant. The San Diego modification of the Dega osteotomy is worth noting because the outer table cut extends completely posterior into the sciatic notch, while the inner table is not disrupted. This makes the osteotomy hinge upon the medial limb of the triradiate cartilage, allowing preferential posterior or anterior coverage depending on where the bone graft is placed. Because neuromuscular hips tend to dislocate in a posterolateral direction, the additional posterior coverage afforded by the Dega or San Diego osteotomies are thought to be of benefit.
.png?lang=en-US)
4. Salvage Osteotomies
The Chiari and Shelf osteotomies are meant to improve femoral head coverage or containment in a non-congruous or subluxated hip joint. In both cases, non-articular bone surface is placed in a supra-acetabular position to act as a buttress to proximal head migration. In the shelf osteotomy, this is heterotopic bone (autograft and/or allograft) that is grafted to the outer table of the ilium. In the Chiari osteotomy the ilium is cut above the acetabulum and the acetabular component is displaced medially, leaving the superior fragment of ilium directly above the hip joint. In both of these cases, the capsule is intended to be left intact to cover the reconstructed bony surface and to help make the articulation with the femoral head more anatomic. There are not meaningful differences between these techniques from a testing point of view, as both have similar indications and choice is likely based off preference and training.
5. OITE Relevance
Test questions for pediatric pelvic osteotomies ask about unique characteristics for one particular osteotomy. At times when there is not surgeon consensus and may be multiple answers, it is generally not tested, or only one of the appropriate answers will appear in the potential answers. Below are some common associations for testing purposes.
- Skeletally mature dysplasia = Bernese PAO (Ganz)
- Skeletally immature DDH = Salter, Pemberton, Dega, (and Steel triple if age >8)
- Pemberton and Dega involve re-shaping/decreasing acetabulum size
- Skeletally immature neuromuscular dysplasia or posterior deficiency = Dega
- Incongruent hip needs coverage = Chiari or Shelf (salvage) osteotomies
Craig Louer, Pediatric Orthopaedic Surgeon, University of North Carolina
POSNA Resident Communications Committee
