Study Guide
Adolescent Blount Disease
Key Points:
• Age of onset is greater than 10 years.• More often unilateral compared to infantile Blount disease
• Although obesity is a risk factor, Blount disease is rarely seen in conjunction with slipped capital femoral epiphysis or diabetes
• Guided growth is likely to fail in children with morbid obesity, severe deformity and in older children with minimal growth remaining
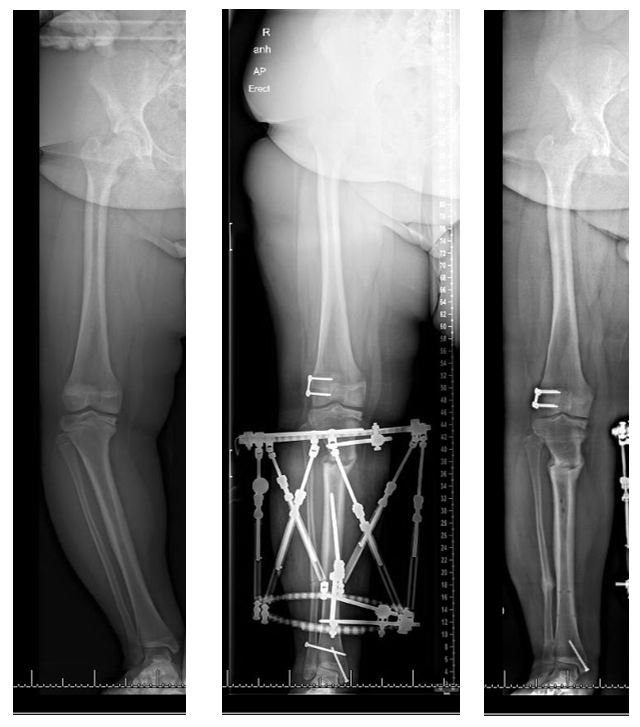
• Deformity is typically multiplanar (varus, increased posterior tibial slope, internal torsion, short) and may benefit from proximal tibial osteotomy, fibular osteotomy, with hexapod circular external fixation
Description:
This condition was first described by Ehrlacher and then popularized by Walter Blount (Blount, 1937). It is usually seen in overweight adolescent children who have involvement of the proximal medial tibial growth plate. This results in a progressive varus deformity of the tibia as well as increased anterior bowing of the tibia (increased posterior tibial slope), internal tibial torsion and shortening of the affected extremity.Epidemiology:
There is scant current epidemiologic data on the incidence or prevalence of adolescent Blount’s disease. In the early 1990s the prevalence in a high-risk adolescent, African-American, obese population was as high as 2.5% (Henderson, 1993).Clinical Findings:
Adolescent Blount disease is also known as late onset Blount disease. The adolescent version of Blount disease is defined as 10 years or greater. These children are frequently obese. Involvement is more frequent in boys and African Americans. Unilateral involvement is more frequent compared to bilateral involvement. (Rivero,2015). Clinically, patients present with progressive bowing of the tibia along with shortening of the affected extremity. They may have medial knee pain and a limp. Physical examination of the knee often demonstrates varus and anterior bowing as well as internal tibial torsion. In severe disease, lateral collateral ligament laxity which may manifest as a thrust in stance phase of gait. Patients with Blount disease frequently have planovalgus feet.
Imaging Studies:
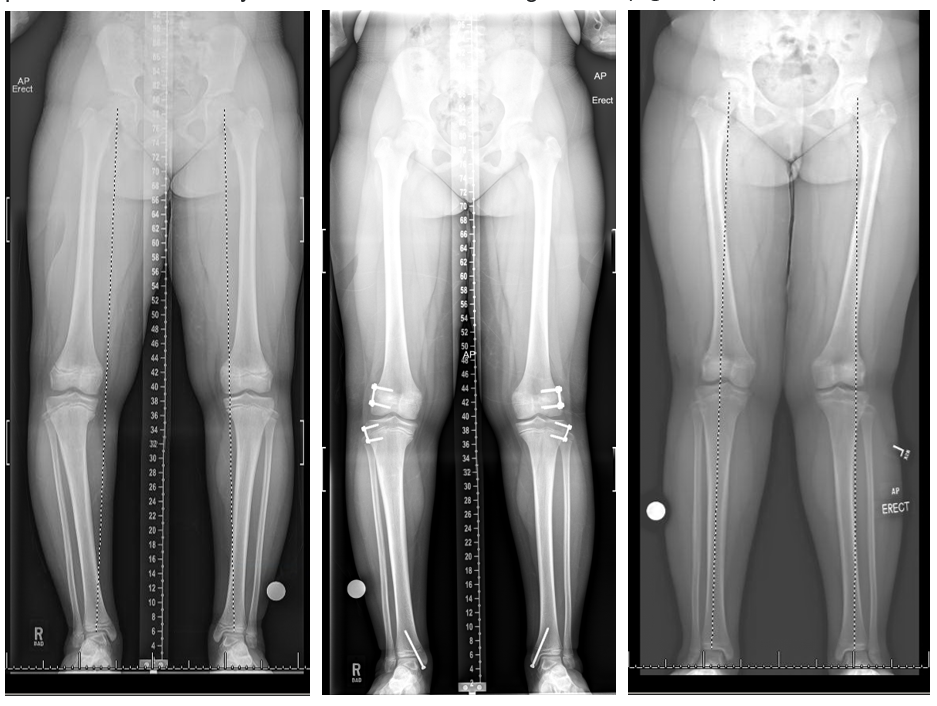
Standing hip to ankle radiographs of bilateral lower extremities should be obtained. The growth plate of the proximal tibia initially may be wider and more irregular medially compared to normal, while later in the disease progression, a bar or sclerosis with early fusion at the medial physis may be identified. There may be changes at the distal femur, commonly varus. The medial proximal tibial angle (MPTA) should be approximately 88°, and decreased MPTA is consistent with varus at the proximal tibia. The posterior proximal tibial angle (PPTA) measured on the lateral view should be 80°, and decreased PPTA is common (procurvatum, increased posterior tibial slope).Internal tibial torsion can be assessed clinically or using a computed tomography (CT) version study. The lateral distal femoral angle (LDFA) should be approximately 87°. The LDFA can be normal, decreased (compensatory valgus) or most commonly increased (in varus). Distal femoral deformity may be a substantial contributor to the overall limb varus alignment (Gordon, 2006). Unlike in infantile Blount disease, depression of the tibial plateau is not seen. The ankles are often in valgus and these patients often have planovalgus feet. Advanced imaging is rarely indicated in this population except for assessment of version.
Treatment:
Treatment of adolescent Blount disease depends on severity and amount of growth remaining.Growth modulation:
Growth modulation may be attempted in patients with mild to moderate deformities and with adequate (ideally more than 2 years) growth remaining. The failure risk with growth modulation may be as high as 66% (Macintosh, 2009). Risk factors for failure include high body mass index and severe deformity (Macintosh, 2009 and Funk, 2016). A higher failure rate may also be seen in patients with lack of adequate growth remaining. It is important to note that some children with Blount disease have advanced bone age compared to that age matched counterparts without Blount disease (Sabharwal, 2013). Assessment of bone age therefore is critical in choosing the correct treatment option. Growth modulation with a tension band plate or similar systems does not correct the internal tibial torsional deformity. Also, if there is a significant limb length discrepancy, this would need to be addressed separately.
Growth modulation of the distal femoral varus as well as distal tibia valgus may be performed concurrently if these deformities are significant. (Figure 2)
Acute correction:
Osteotomy with acute correction and internal or external fixation may be an option for mild deformity of the proximal tibial and distal femur. An oblique plane osteotomy may be utilized to correct not only the proximal tibial varus but the internal tibial torsion seen in many of these patients. Alternatively, a lateral closing wedge osteotomy or a medial opening wedge osteotomy may also be performed. Fixation may be achieved using internal or external fixation.
Gradual correction: This is often the preferred mode of correction in patients with significant deformity as well as LLD as an external fixator has the advantage of potentially correcting the deformities in all three planes as well as lengthening the tibia in patients with significant limb length discrepancy. (Figure 3) Overcorrection of the tibial rotation should be avoided as patients with planovalgus feet and external tibial torsion (resulting from overcorrection) can develop gait abnormalities secondary to lever arm dysfunction.
Concurrent treatment of the distal femoral varus and distal tibial valgus may be needed. (Gordon, 2005). (Figure 3)
Complications:
Growth modulation may be complicated by failure of correction or incomplete correction. Guided growth implants may be more likely to break in the setting of obesity which is common in Blount disease, or prolonged implantation which may be required in the setting of severe deformity. Solid screws and stainless steel implants should be strongly considered. Osteotomy may be complicated by compartment syndrome, prophylactic osteotomy is recommended. Osteotomy may be complicated by delayed healing, non-healing, over or under correction. Failure to treat Blount disease may result in joint instability, gait deterioration, early joint degeneration and pain.Related Videos:
References:
1. W. P. Blount. Tibia vara: osteochondrosis deformans tibiae. Journal of Bone and Joint Surgery, 1937, 19: 1-29.2. Funk SS, Mignemi ME, Schoenecker JG, Lovejoy SA, Mencio GA, Martus JE. Hemiepiphysiodesis Implants for Late-onset Tibia Vara: A Comparison of Cost, Surgical Success, and Implant Failure. J Pediatr Orthop. 2016 Jan;36(1):29-35.
3. Gordon JE, Heidenreich FP, Carpenter CJ, Kelly-Hahn J, Schoenecker PL. Comprehensive treatment of late-onset tibia vara. J Bone Joint Surg Am. 2005 Jul;87(7):1561-70.
4. Gordon JE, King DJ, Luhmann SJ, Dobbs MB, Schoenecker PL. Femoral deformity in tibia vara. J Bone Joint Surg Am. 2006 Feb;88(2):380-6.
5. Henderson RC, Kemp GJ, Hayes PR. Prevalence of late-onset tibia vara. J Pediatr Orthop. 1993 Mar-Apr;13(2):255-8.
6. McIntosh AL, Hanson CM, Rathjen KE.: Treatment of adolescent tibia vara with hemiepiphysiodesis-risk factors for failure. J Bone Joint Surg Am. 2009 Dec;91(12):2873-9.
7. Montgomery CO, Young KL, Austen M, Jo CH, Blasier RD, Ilyas M. Increased risk of Blount disease in obese children and adolescents with vitamin D deficiency. 2010 Dec;30(8):879-82.
8. Rivero SM, Zhao C, Sabharwal S. Are patient demographics different for early-onset and late-onset Blount disease? Results based on meta-analysis. J Pediatr Orthop B. 2015 Nov;24(6):515-20.
9. Sabharwal S, Sakamoto SM, Zhao C. Advanced bone age in children with Blount disease: a case-control study. J Pediatr Orthop. 2013 Jul-Aug;33(5):551-7.

