Study Guide
AC Joint and Clavicle Injuries
Key Points:
- Pediatric acromioclavicular (AC) injuries are typically physeal injuries or occult fractures and not ligament injuries, and AC dislocations have been referred to as “pseudodislocations. ”
- Rule out atraumatic distal clavicle osteolysis, a repetitive stress injury in young athletes who do high level upper body weight training.
- Pediatric clavicle fractures can usually be managed nonoperatively
- Surgical indications for adolescent clavicle fractures are currently controversial.
Description:
The distal clavicular physis ossifies around age 18 years, closing soon after beginning ossification. The main AC joint stabilizers include the AC capsule, with the superior and posterior portions contributing most to stability, coracoclavicular (CC) ligaments (conoid and trapezoid), and coracoacromial (CA) ligament. True AC dislocations in the pediatric population are rare. Instead, the medial clavicular fragment peels off from the periosteal sleeve which maintains its attachments to the coracoclavicular and acromioclavicular ligaments. True AC joint injuries occur more often in men, in their 20s, and are incomplete injuries.Epidemiology:
The clavicle is the first bone to begin ossification and the last to complete ossification. Clavicle fractures are common in pediatric populations, accounting for 8-15% of all skeletal injuries in children and 33% of all shoulder girdle injuries.Clinical Findings:
Tenderness and deformity at the distal clavicle or mid-shaft of the clavicle may be seen. Ecchymosis and edema may be present given the traumatic mechanism of injury. Pain and swelling near the AC joint in the absence of injury could indicate infection or tumor. Sharp bone edge or severe deformity may tent the skin and put it at risk. A careful neurovascular exam must be completed given local anatomy of the mid-shaft of the clavicle. Tenderness to palpation and pain with cross arm testing may be indicative of AC joint injury. O’Briens test may be used to differentiate AC joint pathology from intra-articular SLAP tear pathology.Imaging Studies:
AP and 45 degree cephalic tilt radiographs are typically used for clavicle evaluation. Due to the complex S shape of the clavicle, displacement is difficult to measure on plain radiographs. Contralateral films may be warranted for comparison. CT is generally not required but may be used to determine exact fracture displacement and angulation measurement, for preoperative planning, or to evaluate nonunions and malunions.AC joints are best viewed on the Zanca view which utilizes 10-15 degrees of cephalad tilt with only 50% penetration of normal shoulder xray. Stress views with 5lbs in each hand may be useful to evaluate AC joint instability. It is necessary to rule out coracoid fractures, with maintained CC interspace as well as distal clavicle osteolysis, which is related to stress overuse in young athletes who do repetitive upper extremity weight lifting.
Treatment:
Nonoperative management has been the mainstay of treatment for AC pseudodislocations and type 1-3 AC dislocations. This includes sling or figure-of-eight braces and gentle range of motion. Given the late physeal closure and high remodeling rate, adolescent patients have been reported to remodel these physeal dislocations.Operative indications for AC pseudodislocations include over 8 years old with greater than 2 cortices displacement. Wire fixation has been shown to result in wire migration and generally should be avoided. Type 4-6 AC joint dislocations are often offered operative intervention given displacement, soft tissue compromise, and risk of long term AC joint arthrosis.
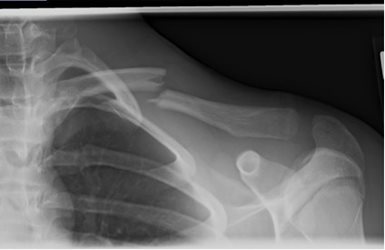

Nonoperative management is the mainstay of treatment for pediatric clavicle fractures. (Figure 2) This most commonly includes sling or figure-of-eight bracing for 2-4 weeks followed by range of motion and return to sports around 8 weeks. Minimally displaced or occult fractures of the distal clavicle may be stable for return to sports as soon as 3-4 weeks. Recent adult literature stating benefits of surgical intervention has called this into question, though no specific surgical indication recommendations have been determined for the pediatric population. Some suggest indications similar to those in the adult literature and include associated neurovascular injury, open injuries or those with skin at risk, fractures with 15-20mm of shortening, 100% displacement, or presence of a comminuted piece hold the main two fracture fragments apart. (Figure 3)

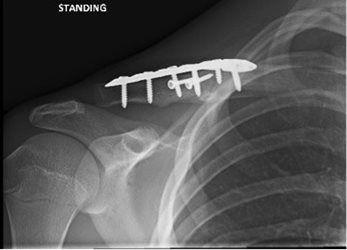
Figure 4 depicts a similarly displaced clavicle fracture in a 14 yo male that acheived successful union with non-operative treatment



These indications are untested in pediatric populations. Reported nonunion rates for pediatric clavicle fractures are generally low and symptomatic malunions are less than 20%. Acute surgical treatment often necessitates a second surgery for removal of implants.
Complications:
Healing rates are very high for AC pseudodislocations. Main complications include activity related pain and mild cosmetic shoulder asymmetry. Chronic AC dislocations can result in chronic pain and instability. Operative complications include implant migration, clavicle or coronoid fracture, osteolysis, loss of reduction, erosion of cerclage material through clavicle or coronoid, AC joint arthrosis, and chronic pain. Clavicle malunion has been shown to result in less than 7 degree range of motion deficit in abduction and less than 8 degrees in flexion, which is thought to be not clinically significant. Shoulder kinematics are affected with greater degree of malunion and displacement, though outcomes of this are unknown in skeletally immature patients. There was no difference in strength testing. Corrective osteotomy can be completed for symptomatic malunions in patient complaining of shoulder ptosis, aesthetic asymmetry, boney prominence, neurologic symptoms or weakness. (Figure 4)


Related Videos:
References:
- Bae DS, et al. Shoulder motion, strength and functional outcomes in children with established malunion of the clavicle. J Pediatr Orthop. 2013;33(5):544-550
- Carry PM, et al. A survey of physician opinion: adolescent midshaft clavicle fracture treatment preferences among POSNA members. J Pediatr Orthop. 2011;31(1):44-49
- Namdari S, et al. Fixation of displaced midshaft clavicle fractures in skeletally immature patients. J Pediatr Orthop. 2011;31:507-51
- Nenopoulos SP, et al. Outcome of distal clavicular fracture separations and dislocations in immature skeleton. Injury. 2011;42:376-380
- Lee SY, et al. What role do plain radiographs have in assessing the skeletally immature acromioclavicular joint?. Clin Orthop Relat Res. 2014;472:284-293
- Pandya N, Namdari S, Hosalkar HS. Dispalced clavicle fractures in adolescents: facts, controversies, and current trends. J Am Acad Orthop Surg. 2012;20:498-505
- Robinson L, Gargoum R, Auer R, Nyland J, Chan G. Sports participation and radiographic findings of adolescents treated nonoperatively for displaced clavicle fractures. Injury. 2015 46(7):1372-6
- Schulz J, Moor M, Roocroft J, Bastrom TP, Pennock AT. Functional and radiographic outcomes of nonoperative treatment of displaced adolescent clavicle fractures. J Bone Joint Surg Am. 2013 95(13):1159-65.

